[ad_1]

For years, Melanie Musson’s friends have marveled at her superpower: staying healthy no matter what germs are making the rounds. Colds and flu felled plenty of Musson’s dormmates in college, but the viruses always seemed to pass her by. “I never got sick once,” she says. “I got about five hours of sleep a night, I finished school in three years, and I worked 30 hours a week throughout. My best friends labeled me ‘the machine.’ ”
Musson’s ironclad immune system also set her apart at her first job. While she was working at an assisted living facility, her co-workers succumbed to a stomach virus that was running rampant. Undaunted, Musson offered to cover their shifts. “There I was, the brand-new employee, getting as much overtime as I wanted. I wasn’t worried that I’d catch [the virus], because it just doesn’t happen.”
While the rest of us battle seasonal flu, chronic allergies, and back-to-back wintertime colds, Musson and other immune masters glide through with scarcely a sniffle — something University of Pittsburgh immunologist John Mellors sees all the time. “People get exposed to the same virus, the same dose, even the same source. One gets very sick, and the other doesn’t.”
Why Do I Get Sick So Often?
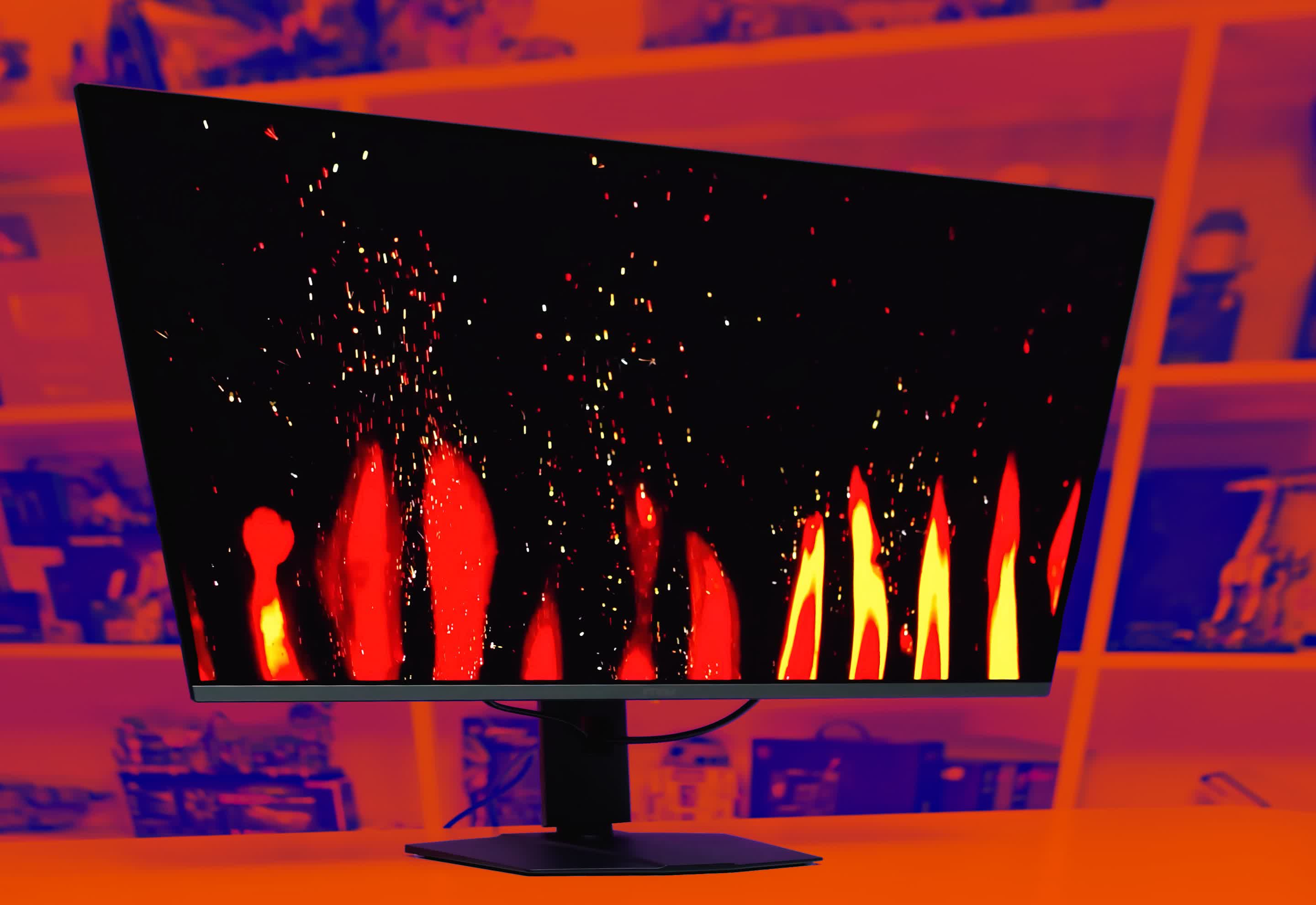
(Credit: ShotPrime Studio/Shutterstock)
Doctors have noted natural variations in the immune response for centuries. New research, however, is starting to illustrate just how your genes, habits, and past disease exposures affect the character and strength of your immune response.
These discoveries are helping to define the parameters of a race in which people like Musson have a head start — and others have much more ground to cover. It’s only natural to wonder: Why do some people always seem to fall on the right side of this equation? And could our own immune systems approach the same level with the right tuneup?
Read More: Chicken Noodle Soup Really Can Help When You’re Sick
How Genetics and Your Immune System Work
The moment a virus, bacterium, or other invader breaches your cells’ walls, your body rolls out a tightly choreographed defense strategy. The main architects of this process are a set of human leukocyte antigen (HLA) genes.
What Are Human Leukocyte Antigens?
HLA genes code for molecules that fine-tune the body’s immune response. They are a key component of the immune system, responsible for presenting antigens to immune cells and triggering immune responses.
How Do HLA Genes Strengthen Your Defense System?
When a bacterium gets into one of your cells, your HLA genes churn out proteins that flag the cell as infected so that specialized immune cells will swarm in to destroy it. Other HLA genes activate cells that rein in the immune response, so it doesn’t destroy more than necessary.
Like fingerprints, everyone’s HLA gene assortment is unique. Your HLA genes give you a broad repertoire of immune defense tactics, but “that repertoire may be great for some microorganisms and lousy for others,” Mellors says. “It’s not like there’s one HLA type that’s highly immune to everything.”
This genetic variation helps explain why you might catch every cold virus going around but haven’t gotten a stomach bug in decades. A Massachusetts General Hospital study found that some so-called HIV controllers — immune stalwarts who don’t develop AIDS from the virus HIV — have HLA gene variants that prompt specialized cells to swarm in and attack proteins key to the virus’ function.
Read More: This Rare Genetic Condition Leads to Cancer After Cancer
What Else Causes Differences In Our Immune Systems?
But your human leukocyte antigens genes aren’t the only ones that shape your immune resistance. The Human Genome Project has identified tens of thousands of gene variants that are more common in people who develop specific diseases and less common in people without these conditions.
Identifying Variants in Gene Disease Links
Flagging these kinds of gene-disease links is a relatively simple matter, says immunologist Pandurangan Vijayanand of the La Jolla Institute for Immunology. After researchers identify a gene sequence that’s linked to disease, however, they need to “figure out what it is actually doing,” says Vijayanand. “How is this change in the sequence impacting the cell or causing the susceptibility [to disease]?”
How Do Proteins Regulate Cell Processes?
To answer this question, Vijayanand and his team are creating what they call an atlas, to catalog which proteins each gene produces and how these proteins change the function of different cell types.
For example, he has identified a gene variant that makes people more prone to asthma — a condition in which the body attacks its own healthy airway cells — by driving high production of proteins that rev up the immune response. Other gene variants appear to help people fight lung tumors by prompting their tissues to produce more T lymphocytes, specialized immune shock troops that kill cancer cells.
Is Immunity Genetically Inherited?
Yes, immunity to sickness can be genetically inherited. While a dizzying number of genetic differences remain to be cataloged, immunologists agree that, in general, these differences help explain why resistance to some pathogens can seem to run in families.
People like Melanie Musson probably get a genetic leg up to some degree — Musson says her mother, father and siblings rarely get sick. Conversely (and unfairly), you might instead inherit a tendency to develop diabetes, recurrent strep infections or autoimmune diseases.
Read More: Can Boosting Immunity Make You Smarter?
What Causes a Weak Immune System?
However anemic or hardy your innate immune arsenal, it supplies only the broad contours of your body’s resistance to threats. Environmental influences fill in the details, from where you live to your sleeping patterns to your history of previous infections.
Genetics and the Immune Response
In a 2015 cell study, researchers studied more than 100 pairs of identical twins and how their immune systems responded to the flu shot. About three-quarters of the differences they saw were driven by environmental factors rather than genetic ones. The differences in twins’ immune systems also grew more pronounced the older they got, suggesting that outside influences continue to shape our immune potential over time.
Childhood Factors and Immune Health
Some of these influences show up in early childhood and may be hard to offset later on. Researchers have long known that children who live on farms are less likely to develop autoimmune diseases like asthma and allergies. An Ohio State University study from July 2019
hints at one reason why: Farm kids have a more diverse array of gut microbes than city kids, and the presence of some of these gut microbes predicts lower frequencies of immune cells that create allergic inflammation. Broad microbial exposure, in short, appears to train the immune system not to overreact to substances like animal dander.
Diseases and the Immune System
But regardless of where you grew up, if you’re unlucky enough to catch certain disease-causing bugs, they can throw your immunity off balance for years. Cytomegalovirus, a relative of the virus that causes chicken pox, stages its attack by reprogramming the human immune system. Some of the virus’ proteins latch onto certain immune cells, interfering with their ability to fight invaders.
Other proteins, according to research from the University Medical Center Utrecht, interfere with the expression of key human HLA genes. And since cytomegalovirus infections are chronic, the resulting immune deficits can go on indefinitely.
Read More: What Stress Does to the Immune System
What Are the Symptoms of a Weak Immune System?
Not everyone’s immune system functions at its best, and a weakened immune system can leave you vulnerable to a range of health challenges. Understanding the symptoms of a weak immune system is crucial for taking proactive steps to bolster your immunity and maintain optimal health.
Frequent Infections
Individuals with a weakened immune system are prone to getting infections more often than others. These infections may also be more severe or challenging to treat.
Uncommon Infections
Weakened immunity can lead to susceptibility to infections that a person with a stronger immune system would not typically contract.
Common Infections
Some common infections associated with a weak immune system include pneumonia, meningitis, bronchitis, and skin infections.
Recurrence
Infections in people with compromised immunity may recur frequently.
Other Health Impacts
Weak immunity can also result in autoimmune disorders, inflammation of internal organs, blood disorders (such as anemia), digestive issues like loss of appetite, diarrhea, and abdominal cramping, as well as growth and developmental delays in infants and children
Read More: Why We Feel So Terrible When We Get Sick
How To Not Get Sick
Naturally, you can’t control where you’re raised or what random pathogens you acquire. But you can control your daily routine, what you put into your body and how you shield yourself against germs. In recent years, scientists have begun a full-fledged push to find out which lifestyle habits actually foster a robust immune system — and which may be more hype than substance.
Diet and Immunity
While the overall picture of how diet shapes immunity is still blurred, new studies do hint at the immune-strengthening effects of certain types of foods.
Garlic, for instance, contains a sulfur compound called allicin, which spurs production of disease-fighting immune cells like macrophages and lymphocytes in response to threats.
(Credit: Lucky_Find/Shutterstock)
Researchers also report that specific bacteria-containing foods — such as sauerkraut, kimchi and kefir — produce an immunologically active substance called D-phenyllactic acid. This acid appears to signal immune cells, called monocytes, to report for duty by binding to a receptor protein on the cells’ surfaces.
When people eat sauerkraut, “very soon afterward, we see in the blood that there’s an increase in the level of this substance,” says Leipzig University biologist Claudia Stäubert. In future studies, she hopes to clarify exactly how the acid affects monocytes’ activity in the body.
Exercise and Immunity
In addition to tweaking their diets, many titans of immunity embark on intense exercise regimens to keep their health robust. “I swim and snorkel year-round in the ocean, up to a mile at a clip, from New England to Miami and a few secluded points in between,” says Baron Christopher Hanson, a business consultant who claims he almost never gets sick.
Studies have shown that moderate exercise reduces the incidence and duration of illnesses like upper respiratory tract infections. And a new study in rats shows that regular exercise changes the prevalence of different types of immune cells, though it isn’t clear how these changes make you less likely to get sick.
Sleep and Immunity
Getting plenty of sleep is one way to boost your immune health: The body preps disease-fighting cells while you’re asleep. (Credit: Realstock/Shutterstock)
Getting your daily quota of shut-eye, however, does seem to boost your immunity. Repea
ted studies show that sleep revs up your immune response, and a recent one from Germany’s University of Tübingen reports that it does so in part by preparing disease-fighting T cells to do their jobs more effectively.
That’s because your body churns out more integrins — proteins that help T cells attach to germ-infected cells and destroy them — while you’re asleep. But while getting more sleep could help snap your streak of winter colds, squirting your palms with hand sanitizer may not.
Regular Hand Washing
In numerous studies, plain old soap and water kills germs better than sanitizer does. “Hand sanitizer is great for alcohol-susceptible bugs, but not all bugs are susceptible,” Mellors points out. What’s more, using sanitizer won’t have any lasting effects on your immunity. The moment you touch another germy surface, your thin layer of protection will vanish.
Read More: Irregular Sleep Schedules Can Lead to Health Risks
What Causes an Overactive Immune System?
An overactive immune system can be just as troublesome as an underactive one — autoimmune conditions like rheumatoid arthritis, multiple sclerosis and allergies all stem from an immune response that’s too forceful and sustained. Champions of immunity tend to credit their daily habits with keeping them healthy.
But many have also lucked into an ideal balance between effector T cells, the frontline immune soldiers that fend off pathogens, and regulatory T cells, which keep the body’s immune arsenal in check so it won’t over-respond to threats.
How To Normalize an Overactive Immune System
To normalize an overactive immune system, one potential approach is to convert T cells in a laboratory setting. Last year, scientists at Kyoto University in Japan and elsewhere described this process as turning effector T cells into regulatory T cells.
Autoimmune episodes “are triggered by antigens binding to [a] receptor on effector T cells,” says molecular biologist Shuh Narumiya, one of the paper’s authors. When Narumiya and his colleagues used an inhibitor chemical to block an enzyme that controls cell development, cells that would normally develop into effector T cells turned into regulatory T cells instead — a tweak that dialed down harmful autoimmune responses in mice.
Could Regulating T Cells Help Autoimmune Conditions?
While not everyone needs such immune fine-tuning, some people could potentially benefit from a treatment based on this technique, Narumiya says. Filling out the ranks of regulatory T cells could someday help keep a range of disabling autoimmune conditions under control.
Regardless of your T cell balance or your immune track record, there’s a hefty dose of serendipity involved each time your immune system faces a threat. You might consider yourself forever prone to the flu or sniffles, but an X-factor — a cross-country move, a dietary tweak, a new therapy — can unexpectedly realign things and boost your immune potential.
The Unpredictable Nature of Immune Health
By the same token, no matter how stalwart your HLA gene arsenal, how sound your sleep or how scrupulous your hygiene, you can end up knocked flat with a nasty bug when you least expect it.
Immune health “is like a gigantic roulette wheel. You throw the ball down and where it lands is a matter of chance,” Mellors says. “You have an encounter with a pathogen, and at the time you get exposed, your front line is not up to snuff.”
Even titans of immunity can have Achilles’ heels — and even immune systems that seem licked at the beginning can pull off unlikely victories.
Read More: Meet Your Lymphatic System: A Key Part of the Immune System
Are Some People Immune to COVID-19?
(Credit: Andrii Vodolazhskyi/Shutterstock)
While some individuals may exhibit resistance, it’s important to note that complete immunity to COVID-19 is rare. Those infected with the virus develop vastly different symptoms.
Some barely feel anything — a scratchy throat, if that — while others spend weeks in the ICU with ravaged lungs, unable to breathe on their own. This wide variation in how people respond to SARS-CoV-2 stems, in part, from each person’s unique genetic and lifestyle factors that affect their immune function.
Genes
Because the novel coronavirus only recently appeared in humans, we don’t know exactly which genetic quirks might make us more susceptible to it. Scientists are now investigating whether other specific genes might give some people higher or lower degrees of protection against the virus.
Age and Immune Health
In some older people, or in those who have underlying immune deficits from chronic conditions, regulatory T cells — which usually keep immune responses under control — do not function normally.
When these people get COVID-19, so-called cytokine storms may cause excessive inflammation in the lungs, leading to life-threatening symptoms. A study conducted by researchers in China found that COVID-19 patients with severe illness had lower levels of regulatory T cells in their bloodstream. Children may be less prone to disabling symptoms because their immune systems are better regulated and they have fewer underlying conditions.
Smoking Habits
SARS-CoV-2 uses a cell surface receptor called ACE2 to enter the cells that line your respiratory tract. New research shows that in smokers, these receptors are more preva––lent in the lungs, creating more potential access routes for the virus. “If you smoke,” says Boston Children’s Hospital immunologist Hani Harb, “the virus will be able to enter more cells in higher numbers.”
Vaccination
With widespread COVID-19 vaccinations, factors influencing vaccine response become important in determining resistance. COVID-19 vaccines come in different forms, but they all do one important thing: They help your body remember how to fight a virus. Think of them like your immune system’s superheroes. These superheroes, called T-lymphocytes and B-lymphocytes, keep a record of how to defeat the virus.
Read More: Children’s Immune Systems Differ From Adults. Here’s What That Could Mean for COVID-19
Frequently Asked Questions
Why Am I Getting Sick so Often?
Frequent sickness can be due to a combination of factors such as genetic predispositions, environmental exposures, stress, poor sleep, diet, and lifestyle habits. Immune system variations, including HLA gene differences, also play a role.
Why Do I Keep Getting Colds?
Constant colds might be attributed to high exposure to cold viruses, weakened immune defenses, or lack of immunity to various cold virus strains. Environmental factors and hygiene practices are also influential.
Why Do I Get Sick Even Though I’m Healthy?
Even healthy individuals can fall ill due to genetic factors, unexpected exposure to pathogens, or temporary dips in immune function caused by factors like stress or lack of sleep.
Does Getting Sick Build Your Immune System?
Getting sick can strengthen the immune system by creating a memory of specific pathogens, aiding in faster and more effective responses in the future. However, it doesn’t guarantee immunity against different pathogens.
Why am I Getting Sick Every Two Weeks?
This could be due to continuous exposure to pathogens, chronic stress, inadequate nutrition, or an underlying health condition that compromises the immune system.
Why Do I Keep Getting Sick Every Month?
Monthly illness might be linked to lifestyle factors, such as stress cycles, diet, or exposure to pathogens in specific environments.
Why Is my Immune System so Weak?
Perceived weakness in the immune system could be due to genetic factors, chronic health conditions, poor diet, insufficient sleep, lack of physical activity, or environmental factors.
What are the Causes of Frequent Sickness?
Frequent sickness can be caused by a combination of factors such as genetic predispositions, environmental exposure, lifestyle habits, previous infections, poor hygiene, underlying health conditions, age, nutritional deficiencies, and psychological stress.
Read More: Does a Runny Nose Mean You Have COVID-19, the Flu, or a Common Cold?
Elizabeth Svoboda is a science writer in San Jose, California. Her most recent book is The Life Heroic: How To Unleash Your Most Amazing Self.
Editor’s Note: This story was updated to clarify that the link between exercise and immunity to illness is fairly well established. We apologize for the miscommunication.
This originally appeared in the July/August issue of Discover magazine as “Titans of Immunity.” Support our science journalism by becoming a subscriber. The story has since been updated by the Discover staff.
Maqvi News #Maqvi #Maqvinews #Maqvi_news #Maqvi#News #info@maqvi.com
[ad_2]
Source link